Any radio discussion of ecigarettes inevitably attracts evangelical callers wanting to tell their story of the miracle they have experienced:
- “As a fortunate survivor of extended tobacco addiction, 40 years of a pack a day, I have not smoked a single bit of tobacco since I started vaping 5 months ago. I was able to finally give up tobacco after failed attempts at cold turkey, patches, and gum as NRT”
- “I know about 200 people in our small town of 3000 that vape, and only about 3 of those still smoke some cigarettes, and those that do have cut consumption by about 90%.” [note here that a recent English analysis concluded “If use of e-cigarettes and licensed NRT while smoking acted to reduce cigarette consumption in England between 2006 and 2016, the effect was likely very small at a population level.”)
As I’ve previously summarised, there are many reasons why such testimonial statements are considered the weakest form of evidence in answering questions about whether ecigs are serious new entrants in the population-wide game of helping smokers to quit.
The obvious problems with individual testimonies are self-selection bias (people with a success story are far more likely to want to enthusiastically proselytise their story than the many who try and fail); lead time bias or “borrowing from the future” (some people who quit would have quit weeks or months later anyway, perhaps on their own or using another approach, thus artificially inflating the apparent importance of the method they used when they quit); and relapse.
Relapse is a major, much studied sequalae to quit attempts. Far more smokers relapse than quit permanently. Across all methods, relapse dominates, with the maximum rates occurring in the first month after an attempt (eg: see table below).
This means that cross-sectional (“snap-shot”) surveys which report findings on what people’s smoking status is on the day they answered the survey questions have major limitations. Many people have inaccurate recall of their smoking and quit attempt histories and many people who report being ex-smokers on the day they answered the question would answer that they had returned to smoking if asked the same question a few weeks or months later.
For example, this study proposed that by 2014, 6.1m Europeans had quit smoking by vaping. But such “big” numbers often do not withstand scrutiny. The 6.1 million number comes from a cross-sectional survey where ex-smokers reported they used to smoke, then used e-cigarettes and now don’t smoke. Were it only that simple. This critique makes the key point that the survey questions would have allowed those who quit for only a short period to say they had stopped, when relapse is a major phenomenon and demands a longer-term view.
The critics also asked:
“… how many of those who claim that they have stopped with the aid of e-cigarettes would have stopped anyway, and how many of those who used an e-cigarette but failed to stop would have stopped had they used another method?”
Randomised controlled trials?
Well conducted randomised controlled trials are considered high quality evidence, but have major problems that make them difficult to generalise to “real world” settings. If you volunteer to participate in a trial, you are likely to have a disposition to want to help science and so will probably be very positive and diligent about following the study protocol – unlike the way many in real world conditions forget to take their drugs or relapse. Trial participants are regularly contacted by study organisers trained in cohort retention strategies. This regular contact can result in trialists wanting to please “the lovely research assistant who calls me up each week” and can artificially increase study group retention rates, again unlike real world use where no such influences occur.
And if you are heavily dependent on nicotine, enrolled in an RCT and allocated to a study arm with placebo nicotine, guess what? Your withdrawal symptoms will quickly let you know that you are not getting any nicotine, so your belief that the nicotine replacement (NRT or ecigs) you hope you are using might do the trick will instantly be in tatters, with undermining consequences for your quit attempt.
For all these (and several other) reasons, the most important forms of evidence about how people quit smoking are longitudinal cohort studies which use high quality participant selection protocols to best ensure that those being interviewed are a representative sample of the smoking population. With smoking cessation, the endemic problem of high relapse back to smoking makes it vital that we take a helicopter view across time of how long transitions in and out of smoking last, long term and permanent quitting, being the ultimate outcome of interest. The large body of evidence we have about relapse heavily underlines that “persistent abstinence” is of far more importance than a former smoker’s smoking status on a particular day, which can change quickly.
In 2018, two particularly important papers were published by US researchers using the longitudinal PATH ( Population Assessment of Tobacco and Health) data set.
Let’s take a close look at what they found.
Coleman B et al, Tob Control 2018;0:1–10. doi:10.1136/tobaccocontrol-2017-054174
This important report on transitions in the vaping and smoking status of a nationally representative cohort of American adults aged 18+ who use electronic cigarettes (EC) provides rich data that greatly advances our understanding of the natural history of EC use.
If we examine the report’s data and consider the net impact of vaping on the critical goals of having vapers stopping smoking and vaping non-smokers not starting to smoke, the findings are very sobering and should give strong reason for pause among those advocating e-cigarettes as a game-changing way of stopping smoking.
The study reported on transitions between participants’ responses at Wave 1 and Wave 2, obtained 12 months later. At Wave 2, of the cohort of 2036 dual users (EC + smoking) only 104 (5.1%) had transitioned to exclusively using ECs and another 143 (7%) had quit both EC and smoking for a combined total of 247 (12.1%) who had persistently quit smoking. Of the 896 exclusive EC users at Wave 1, 277 (30.9%) had stopped vaping at Wave 2.
So together, 524 out of the 2932 EC users (17.9%) followed from Wave 1 might be considered to have had positive outcomes at Wave 2 (ie: quitting smoking and/or quitting EC).
The other side of the coin however, shows that of the 2036 dual users at Wave 1, 886 (43.5%) relapsed to using cigarettes exclusively. In addition, among the 896 exclusive ECusers from Wave 1, 109 (12.2%) had stopped vaping and were now smoking, with another 121 having resumed smoking as well as using EC (i.e. became dual users). Importantly, 502 of 896 (56%) exclusive e-cigarette users were those who had never been established smokers prior to using e-cigarettes. Alarmingly, of these 502 adults, 120 (23.9%) progressed from using only e-cigarettes to either dual use (54 or 10.8%) or smoking only (66 or 13.2%).
Taken together, 886 dual users in Wave 1 relapsed to become exclusive cigarette smokers in Wave 2, and 230 exclusive vapers in Wave 1 took up cigarette smoking in Wave 2 (dual use or exclusively cigarettes). Undoubtedly, these should be considered as negative outcomes.
The table below shows that for every person vaping at Wave 1 who benefited across 12 months by quitting smoking, there were 2.1 who either relapsed to or took up smoking. Most disturbingly, in this adult cohort nearly one in four of those who had never been established smokers took up smoking after first using EC. Concern about putative gateway effects of ECs to smoking have been dominated by concerns about youth. These data showing transitions from EC to smoking in nearly a quarter of exclusive adult EC users with no histories of established smoking should widen this debate to consider adult gateway effects too.

By far the largest proportion of those with negative outcomes are those dual users who relapsed to smoking (886 or 43.5% of dual users). As the authors noted in their discussion, many of these were infrequent EC users, possibly involved in transitory experimentation at Wave 1. If we add the 902 who were still dual using at Wave 2, then 1788 of 2036 dual users (87.8%) in this sample might be said to have been held in smoking (dual using or exclusive smoking) 12 months later compared to 12.1% dual users who may have benefited by using ECs.
Commercial interests in both the tobacco and EC industries would be more than delighted with these findings. However, from public health harm reduction perspective these results argue against EC being a revolutionary effective harm reduction strategy, and point to their far stronger potential to both recruit smokers and hold many smokers in smoking.
Benmarhnia T et al American Journal of Epidemiology 2018 DOI: 10.1093/aje/kwy129
In a second paper using the PATH data, the authors considered persistent abstinence (not using tobacco for more than 30 days). The red highlighted section of the table below shows that those smokers who used ecigs (called ENDS in the table) had the worst persistent abstinence all-tobacco quit rates of any group in the cohort (5.6% of those who were vaping at the Wave 1 survey and 3.7% of those who too up vaping between Wave 1 and Wave 2). By far the most successful all-tobacco quit rate was for “no aid used” (ie cold turkey or unassisted cessation) with 12.5%.
When we multiply these quit rates by the numbers of smokers using each quit method, the yield of persistent quitters is even starker (see the second table below derived from the data in the table immediately below).

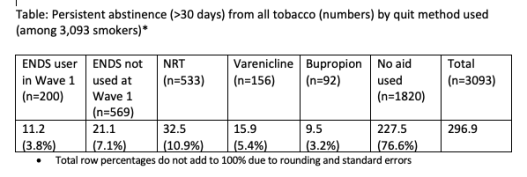
So in this major national cohort of US smokers, not only did EC use produce the lowest rate of persistent abstinence from tobacco use after one year compared to all other quit methods, but EC’s contribution to population-wide tobacco abstinence was utterly dwarfed by all other methods (10.9% v 89.1%). The much-denigrated and neglected unassisted cessation approach quietly ploughed on, continuing its massive historical dominance of how most ex-smokers quit, contributing 1.5 times more quitters than all other methods combined.


Simon, I think there is a selection bias of e-cig proponents who are involved in the e-cig industry. About 18 months ago I was putting a list of e-cigarette industry folks together for ANR. So I looked at a bunch of the e-cig cheerleaders responding to Facebook posts or comments on newspaper articles and some scientific articles. I tracked these people on social media and LinkedIn. Many of the e-cig cheerleaders who appeared in comments had a connection to the industry. They were part of one of the front groups are they actually owned or worked in vape shops.
Joel Dunnington MD, FACR, 1981 Hunters Cove, New Braunfels,TX 78132 (281) 387-6770 jsdunnington@gvtc.com Sent from my iPad
>
LikeLike
Excellent review, Professor. As your quitting method productiveness table indicates, despite the government’s own PATH data screaming the answer, the NIH, FDA and CDC continue their three-decade cover-up of quitting’s most fundamental question: how do the vast majority of ex-smokers successfully arrest their chemical dependence upon nicotine?
Although contrary to both pharma’s and the e-cig industry’s economic interests, smokers deserve the truth. As suggested by a number of studies (most recently Weaver SR 2018 PLoS One), nicotine weaning schemes, in all forms, are significantly less effective in real-world quitting than abrupt nicotine cessation.
What’s needed is richer population level quitting data. Knowing that most smokers quit cold turkey, why does the PATH survey ask multiple questions about other quitting methods yet fail to ask if the quitter’s last attempt was cold turkey: the abrupt and complete end of use of all nicotine or tobacco products, without use of any quitting medication?
Look closely at the U.S. Department of Health’s 944 page 2018 PDF version of the U.S. Population Assessment of Tobacco and Health (PATH) survey (https://whyquit.com/studies/PATH-survey-2018.pdf). In fact, search the entire survey for any questions about cold turkey, abrupt cessation or unaided or unassisted quitting. Now search for questions about the nicotine patch, gum, lozenge, Chantix, Zyban or e-cigarettes.
Why zero inquiry about cold turkey while filled with questions about other methods? Because a complete and accurate quitting picture would devastate pharma’s cessation financial interests, demolish the Food and Drug Administration’s quitting product approval reputation, and suggest that the CDC has spent three decades promoting failure, relapse and disease.
Frankly, I submit that HHS is into pharma’s sham “double your chances” mantra way too long and deep to come clean. But ask yourself, if the government remains unwilling to provide smokers with a full and honest real-world quitting picture, how can it be trusted to tell kids the truth about vaping?
John R. Polito
Nicotine Cessation Educator
LikeLike
A person who relapses to exclusive smoking should not be seen as a negative for vaping. Just like other forms of smoking cessation methods, including cold turkey method, not all approaches work to help ‘every’ smoker.
The negatives for ecigs are those regarding
i) people taking up vaping without having smoked previously
ii) people taking up vaping without having smoked previously and moving onto smoking
iii) Dual-use
But I’m still not convinced that ‘long term’ dual-use is as prevalent as the current results suggest. Both studies failed to implement sufficient qualifiers to weed out those subjects who may have been up-playing their use of vaping.
44.3% maintained dual use
43.5% discontinued e-cigarette use and maintained cigarette
I think with improved questioning to ensure that a person really is using their device (such as asking them how much money they spend on vaping materials per month), you’ll see that 44.3% drop, and the 43.5% rise.
But the issue of people taking up vaping without previously being smokers, and particularly those who transition to exclusive smoking (i.e gateway) is a far more serious concern, and a justification for strict regulation on marketing.
LikeLike
Ben, I don’t buy your premise at all that relapse should not be seen as a negative in assessing the effectiveness of a strategy for smoking cessation. The main considerations in thinking about any method when the principal outcome is the net number of permanent ex-smokers delivered after the strategy is used are:
* uptake of the method (so unassisted is way, way out in front here; while a requirement to attend multiple counseling sessions at a clinic or forking out hundreds of dollars for some flaky strategy like “laser therapy” is (thankfully) at the other end. Vaping scores quite well here.
* propensity for the user to relapse (the data in my piece show lots of relapse & enduring dual use with vaping)
* willingness of smokers to give the strategy further attempts (I’ve published several papers looking at why unassisted is so popular and “rsspected” by smokers. Pretty sure there are not too many repeat varenicline users, and that many who shell out $$ for vaping gear put them in the drawer shortly afterwards).
Consideration of all three considerations against the simple question asked of permanent ex-smokers “what strategy did you use on your final, successful.quit attempt?” shows the true contribution of any strategy to the goal of population-wide cessation.
The smoking cessation literature is spilling over with faux-jubilant claims for the “success” of various strategies which are often measured only short periods out from quit attempts.
By the way, I’ve decided that I will from now on only publish comments on this blog from people who sign their full name. So no more from “Ben” or any fake names.
LikeLike
Pingback: What are the limitations of the randomised controlled trial of ecigs v NRT, just published in NEJM? | Simon Chapman AO
Pingback: The Canadian canary in the teenage vaping coalmine – Southeast Asia Tobacco Control Alliance