When you ask vapers why they vape, different answers are typically given by new experimental vapers and those who have been doing it for longer. Curiosity, the attraction of flavours and lower price are often top of mind in novices. But optimistic harm reduction beliefs are often given by committed vapers.
The twin pillars of vaping advocacy are that vapes have a risk profile that is as near as you can get to being utterly benign, and that they are peerless as a way of quitting smoking. I’ve looked at the latter argument here.
In this blog I’ll revisit 10 articles of faith about the safety issue.
- “Vaping is 95% less dangerous than smoking”
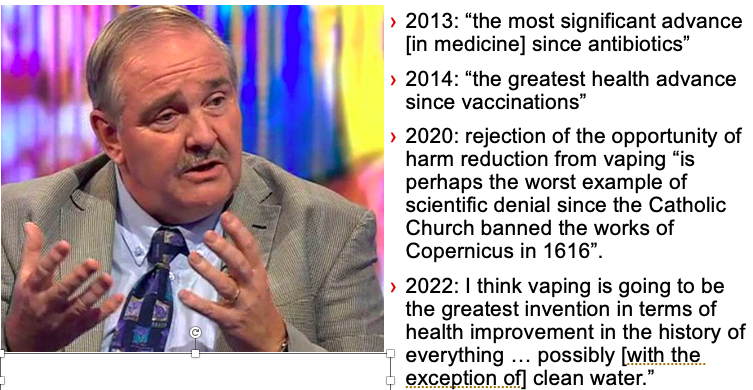
This trite factoid enjoyed massive sunlight for a few years after a 2014 meeting in which it was conjured. I took a close look at its discredited origins in this 2019 blog on the dirty dozen myths about vaping and again with others in this review in the American Journal of Public Health in 2020. Today it is richly deserved future museum piece alongside the greatest hits of the hyperbole king of vaping impact, Britain’s David Nutt.
2. Significant levels of vaping have been around now in Australia for some 10 years. If it was dangerous, where are all the bodies?
Daily vaping rates in Australia increased sevenfold between 2016-2023 from 0.5% (100,000) in 2016 to 3.5% (700,000 people) in 2022–2023. So there are big numbers out there. Should we therefore be seeing evidence of declining deaths from smoking if so many are vaping these “extraordinarily successful” quit smoking aids? No. So when might that start being seen?
Smoking-caused chronic diseases like lung and cardiovascular disease and cancer have latency periods between first exposure and onset of symptoms and formal diagnosis of these diseases. This can vary with age of smoking commencement, duration of smoking and sex. These periods are uncommonly as soon as 15 years but much more likely to be 45+ years.
Current smokers are often diagnosed at a younger age (median ~63y) compared to former smokers (median ~69y). The overall average age for all lung cancer patients (including non-smokers) is typically around 70–72ys. So if smoking commences at ~15, latency periods range from 48-57 years (reference).
If chronic vaping also proves to cause chronic disease, we would not expect to see clear population level evidence of this until around 2050-60.
3. Vaping exposes you to particulates comparable to breathing steam from a kettle in your kitchen
The tobacco industry has decades-long form in trying to trivialise the harms of smoking. This priceless industry document from 1984 was a 20 page aide memoir for industry spokespeople being interviewed by the media about the harms of smoking. It’s not hard to imagine its genesis: “ok team, I want you to find as many things that can cause any sort of health problem that we can rattle off to interviewers who say smoking is harmful. Long hair, hot soup, hobbies. Find us more!
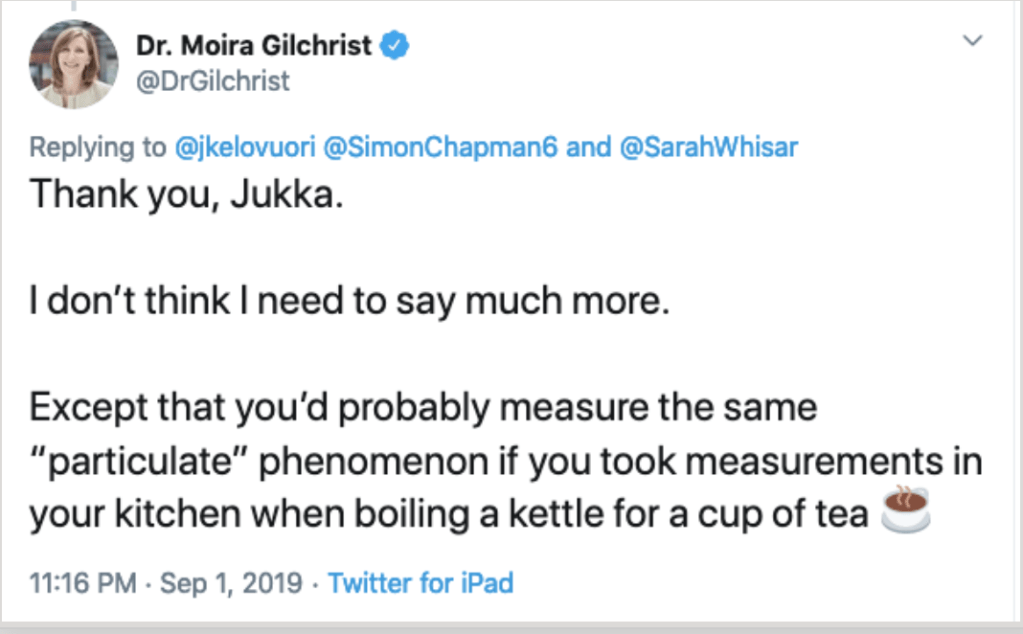
Thirty five years later, Moira Gilchrist, today Chief Global Communications Officer at Philip Morris International, echoed the same thinking when ridiculing silly people who worry about particulate matter exposure from vapes.
4. Flavour chemicals in vapes are just “food grade” chemicals – so nothing to worry about, folks!
Any toxicology undergraduate understands that the route of exposure or administration of a drug or chemical is fundamental in understanding its risks and benefits.Science journalist Dr Heather Goldstone put it beautifully like this (at 11m10to 24m50)
“It doesn’t take someone with an advanced degree in toxicology to understand that drinking water is different than breathing water”.
So swallowing a chemical may present a whole different risk profile to injecting, inhaling or having skin contact with the same chemical. In this blog, I looked at what the peak flavouring and extracts manufacturing association (FEMA)) in the US had to say about inhaling vapourised flavourants.
Here was an industry which earns its fortune from food, beverage and perfume smells and flavours which stood to earn gazillions more if toxicology gave the green light to adding flavourants to vapes. But twice (in 2013 and again in 2020) FEMA red-lighted the entire idea:
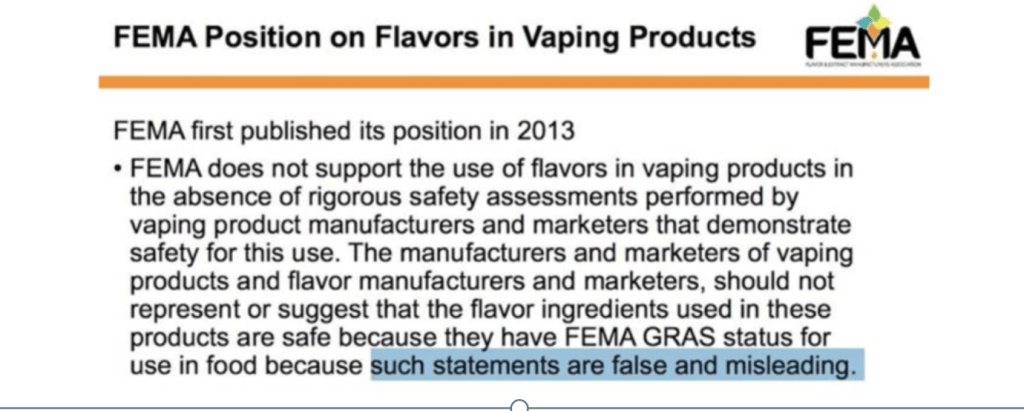
This has made zero impression with vaping advocates who cannot see beyond flavours being a major attractant for vaping. That’s the only myopic question they ask in their evangelical zeal.
In this 2020 blog, I examined the obvious question of why there is no inhalable pharmaceutical product anywhere in the world registered with a government drug regulatory authority which is flavoured. There’s no such thing as flavoured Ventolin (salbutamol) because flavours are totally unnecessary to the therapeutic action of salbutamol. People with asthma do not sign petitions demanding mango or watermelon flavours in their puffers. But vaping advocates will tell you again and again “nothing to worry about” – go ahead and try any one of these beguiling thousands of flavour chemicals, you suckers. Vaping is sooo important, it’s beyond being tied up in the regulations that all therapeutic goods have to meet.
5. “The liquid excipient propylene glycol used in vape liquid is harmless to breathe”
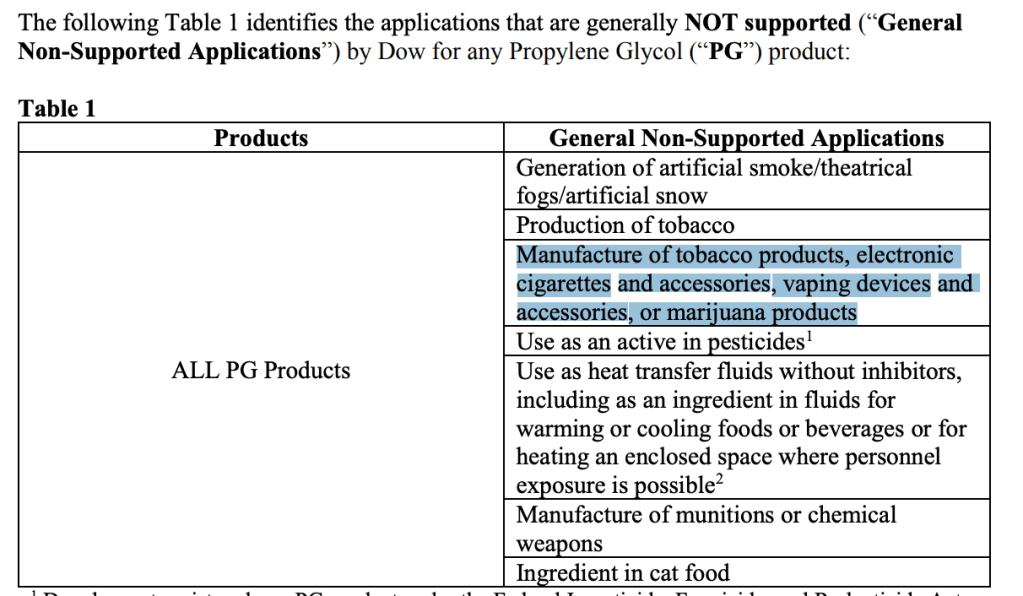
Nicotine in vapes is mostly infused in liquid propylene glycol (PG), along with nicotine, flavourings and temperature control chemicals. When a vape is inhaled, a metal coil in the vape heats this mixuture to 300o Celsius.
Dow Chemical, a major manufacturer of PG in 2019 explicitly named PG in vaping devices and accessories as a “non-supported application”. With the vast earnings potential for Dow in embracing PG in vapes, clearly the risk exposure to the company in doing so must have been assessed as massive.
6. Vaping liquids have cooling agent chemicals added to them to mask harshness
It’s not just PG, flavouring chemicals and nicotine that is added to the brew in vapes. University of Wollongong researchers detected the synthetic cooling agentWS-23 ((N-ethyl-p-menthane-3-carboxamide) in often high concentrations in all disposable vapes they tested. They noted that cytotoxicity studies have found that concentrations of WS-23 below those observed in e-liquids produced adverse effects in cell viability assays.
7. Heavy metal in your lungs, not just in your ears
Heated metal coils in vapes have been shown to shed micro particicles of heavy metals which are inhaled into the lungs.Korean researchers found e-cigarette users exhibited significantly higher serum concentrations of heavy metals than non-smokers. Lead levels were 10 % higher, mercury levels 13.7 % higher and cadmium levels were 61.4 % higher Cigarette smokers demonstrated elevated levels of these metals compared to non-smokers, but had generally lower levels than e-cigarette users.
8. Nicotine levels in vapes are not very addictive
Alex Wodak the tireless Australian vape promoter, says hand-on-heart that “vaping is not terribly addictive”. So consider this recent ABC video at 2m50s where a vaper says he goes through one 5000 puff disposable vape every four days and vapes “first thing in the morning and last thing at night” That’s 1,250 deep lung bastings every day. He’s vaped for four years. So that’s 1.825 million puffs pulled deep across the pink lungs of his mouth, throat and lungs across that time. Not terribly addictive. Yeah, right.
In this observational study of vapers allowed to vape ad libitum (ie as much or as little as they liked), for 90 minutes using their own vaping equipment, the median number of puffs taken over 90 minutes was 71 (i.e. 0.79 puffs per minute or 47.3 per hour). If a person vaped for 12 hours a day at that rate (generously allowing 12 hours for sleep and periods of non-vaping), this would translate to 568 puffs across a 12 hour day or 207,462 times in a year.
But in the ABC video we have a current vaper probably using a vape with five-fold higher nicotine dose than earlier generations of vape.
9. “Nicotine in the doses people get from vaping is all but benign”
The sine qua non of smoking is nicotine. Marketing flashes in the pan like nicotine free herbal cigarettes have all been total market failures because smokers smoke to re-dose themselves with nicotine. The industry fiercely resists proposals for mandated nicotine-free cigarettes, from similar concerns. The industry and its supporters for decades publicly denied nicotine was addictive. After oceans of its internal documents showed this to be an elaborate collusion to stall regulation and reassure the public, it changed its tune.
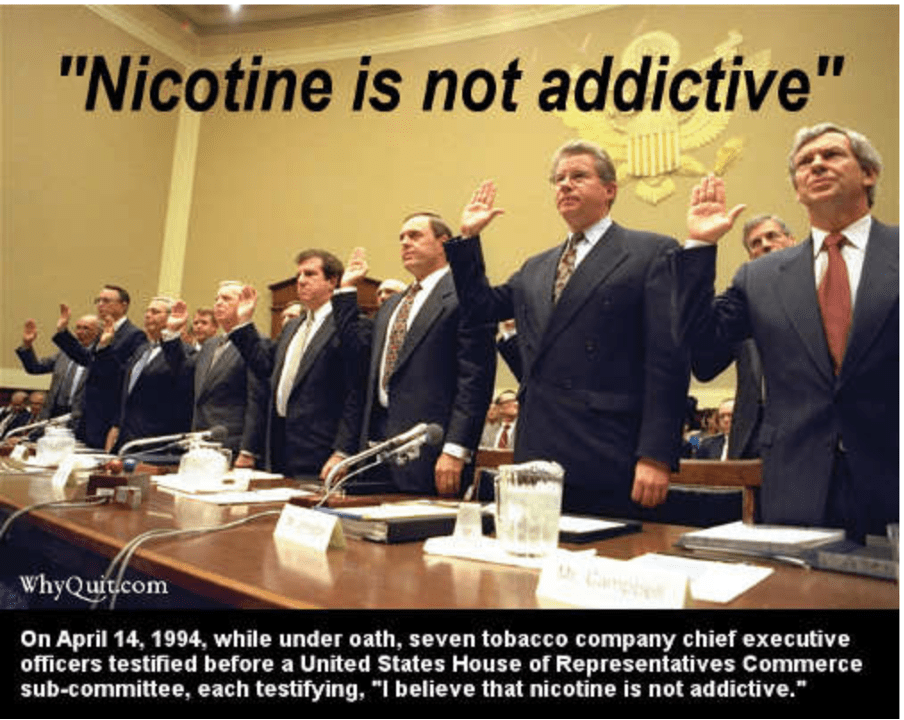
The chorus then changed to “well yes, it is addictive but its harms have been demonised and besides, it’s pleasurable!”. In 2019 I compiled this selection of research about concerns with nicotinepublished in notable journals including Nature Reviews Cancer, Lancet Psychiatry, American Journal of Psychiatry, Mol Cancer Res, Critical Reviews in Toxicology, Carcinogenesis, Mutation Research, Int J Cancer, Apoptosis and Biomedical Reports. These concerns are seldom mentioned by those who recite Michael Russell’s dictum that “People smoke for the nicotine but they die from the tar” as a talisman against any expressed concerns about nicotine.
I’ve also listed numerous recent reviews of the emerging evidence about vaping and precursors of respiratory and cardiovascular disease. This evidence hardly describes an assessment of vaping as a benign practice akin to inhaling steam in a shower or having a couple of cups of coffee a day, analogies we hear used by vaping advocates.
Vaping cheer leader psychologist Peter Hajek said in 2013 “Nicotine itself is probably safer than caffeine ….The case for regulating e-cigarettes as a pharmaceutical product is on a par with regulating coffee.”
No nations regulate coffee, while as at 2021, 37 nations had banned vapes and 73 regulated sales. What do they know that old mate Peter doesn’t?
10. Nicotine is “pleasurable”
In this piece in The Conversation, I looked at the nature of the pleasure that smokers claim for smoking. Just as we all get pleasure from the end of a terrible movie when we are finally able to escape from the middle of a row in the cinema, or from codeine when it works to quell a bad toothache, I argued that nicotine’s reputation for pleasure is mostly about each puff subtly relieving the onset of nicotine withdrawal sensations:
“Smokers know from the earliest days of their addiction these feelings can disappear within a few seconds as the nicotine is rapidly transported from their lungs to their brains where dopamine is released and experienced as pleasurable.
Smokers often insist the pleasure from this release can somehow be experienced independently of the pleasures of the nicotine withdrawal symptoms rapidly dissipating.
So what is the “pleasure” being experienced here? When you have a toothache and this is relieved by a strong analgesic, your mood can quickly elevate as the codeine begins to work.
The argument that smoking and inhaling nicotine is “pleasurable” is a bit like saying being beaten up every day is something you want to continue with, because hey, it feels so good when the beating stops for a while.”
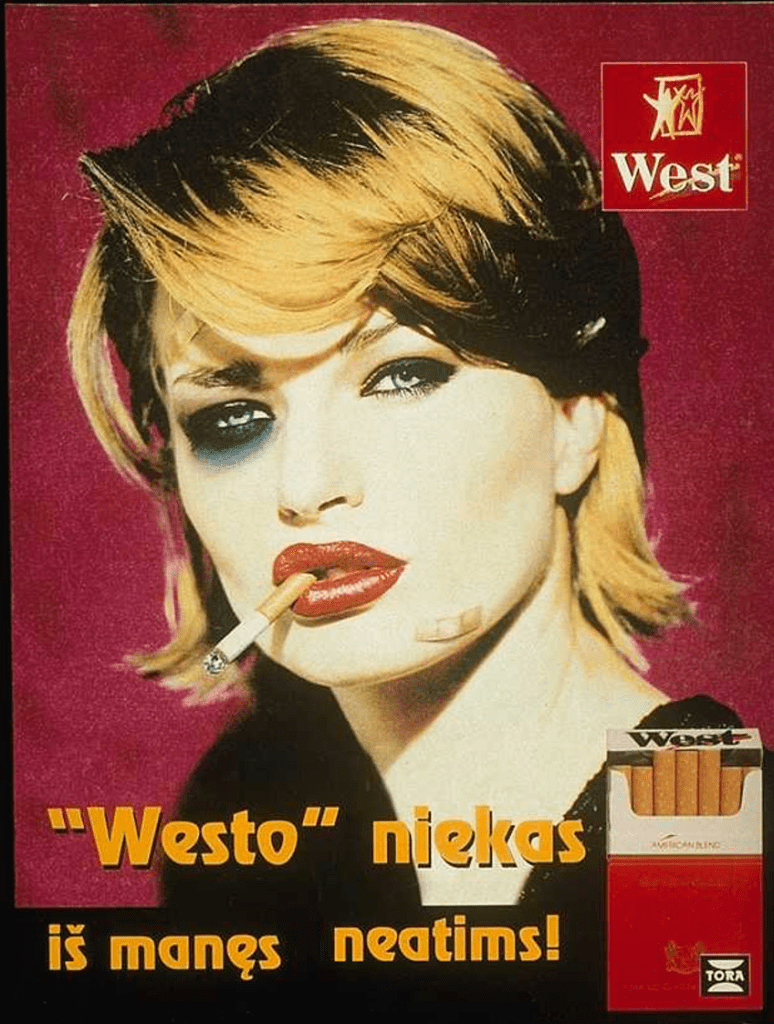
Latvian ad for West cigarettes.
Translation: Westo -This shit won’t take it away from me.(ie I’d rather be beaten up than stop smoking West)
Also in this series
Vaping theology: 1 The Cancer Council Australia takes huge donations from
cigarette retailers. WordPress 30 Jul, 2020
Vaping theology: 2 Tobacco control advocates help Big Tobacco. WordPress 12 Aug, 2020
Vaping theology: 3 Australia’s prescribed vaping model “privileges” Big Tobacco WordPress Feb 15, 2020
Vaping theology: 4 Many in tobacco control do not support open access to vapes because they are just protecting their jobs. WordPress 27 Feb 2021
Vaping theology: 5 I take money from China and Bloomberg to conduct bogus studies. WordPress 6 Mar, 2021
Vaping theology: 6 There’s nicotine in potatoes and tomatoes so should we restrict or ban them too? WordPress 9 Mar, 2021
Vaping theology: 7 Vaping prohibitionists have been punished, hurt, suffered and damaged by Big Tobacco WordPress 2 Jun, 2021
Vaping theology: 8 I hide behind troll account. WordPress 29 Jun, 2021
Vaping theology: 9 “Won’t somebody please think of the children”. WordPress 6 Sep, 2021
Vaping theology: 10: Almost all young people who vape regularly are already smokers before they tried vaping. WordPress 10 Sep, 2021
Vaping theology: 11 The sky is about to fall in as nicotine vaping starts to require a prescription in Australia. WordPress 28 Sep, 2021
Vaping theology: 12 Nicotine is not very addictive WordPress 3 Jan 2022
Vaping theology 13: Kids who try vaping and then start smoking,would have started smoking regardless. WordPress 20 Jan, 2023
Vaping theology 14: Policies that strictly regulate vaping will drive huge
numbers of vapers back to smoking, causing many deaths. WordPress 13 Feb, 2023
Vaping theology 15: The government’s prescription vape access scheme has failed, so let’s regulate and reward illegal sellers for what they’ve been doing. WordPress 27 Mar 2023
Vaping theology 16: “Humans are not rats, so everybody calm down about nicotine being harmful to teenage brains”. WordPress 13 Jul, 2023
Vaping theology 17: “Vaping advocates need to be civil, polite and respectful” … oh wait. WordPress 3 Oct, 2023
Vaping theology 18: Vaping is a fatally disruptive “Kodak moment” for smoking. WordPress Oct 30, 2023
Vaping theology 19: Vaping explosions are rare and those who mention them are hypocrites. WordPress 17 Nov, 2023
Vaping theology 20 : Today’s smokers are hard core nicotine dependent who’ve tried everything and failed – so they need vapes. WordPress 14 Dec, 2023
Vaping theology 21: Australia’s prescription vapes policy failed and saw rises in underage vaping and smoking. WordPress 10 Jan, 2024
Vaping theology 22: “Prohibition has never worked at any point for any other illicit substance”. WordPress 17 Mar 2024
Vaping theology 23: “84% of the Australian public are opposed to the way the government will regulate vapes” WordPress 2 Apr, 2024
Vaping Theology 24: “Tobacco control advocates are responsible for vape retail store fire bombings and murders. WordPress 27 May, 2024