I have a dear friend who has lived with strong pain every day and night for over a decade. Following extensive damage to her spine from osteoporosis, she was advised to have a spinal fusion operation, on threat of needing a wheelchair for the rest of her life. She has a metal “cage” supporting her lower spine but pain fills her life. More often than not, she wakes several times a night and gets some relief from hot showers. Pain relieving drugs are a daily part of her life. Globally, millions of people live with unremitting pain. If you are in pain, it dominates your life.
I originally published this piece (below) in the Sydney Morning Herald, 18 September, 1999. It was republished in a collection of 71 of my writings on health Smoke Signals, in 2016.
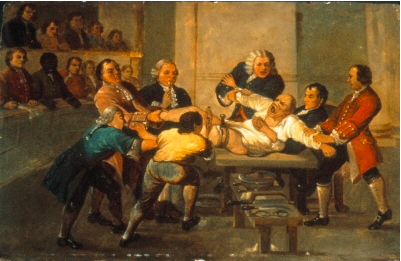
In 1809, 47 year old Jane Crawford risked scalping and the tomahawk to ride her horse 60 miles in four days to the practice of Dr Ephraim McDowell in Danville, Kentucky. Mrs Crawford’s ovarian tumour was giving her unremitting, labour like pain. While several men held her arms and legs, and she recited psalms, McDowell took 25 minutes to cut a 14cm incision in her lower belly, remove a 1.2kg tumour and then sew her up with interrupted sutures. Outside the house, an angry and incredulous mob not unlike those who would today seek to close heroin injecting rooms that minister to a different sort of pain, waited ready to lynch McDowell should his patient die. Five days later she was out of bed and lived for another thirty years.
McDowell’s pioneering operation and his patient’s courage are historical landmarks in the annals of surgery.
While opium and cocaine have been used since antiquity for pain relief, it was not until 1846 when Thomas Morton first used ether to anaesthetise a patient for a tooth extraction that lengthy and detailed surgery more subtle than crude hacking could be performed under general anaesthesia. The next year, chloroform was used for the first time to relieve pain in childbirth and went on to become the anaesthetic of choice for more than a century. Today, pain management specialists estimate that more than 90% of postsurgical, post-trauma and cancer pain can be fully relieved, and 75% in chronic, non-cancer pain such as arthritis. Thirty years ago, these figures hovered around 10%. Worldwide though, only half those suffering from these conditions have access to services and drugs which can provide this relief.
Proust wrote that “Illness is the doctor to whom we pay most heed: to kindness, to knowledge we make promises only; pain we obey.” People in pain are preoccupied by the experience. Pain bulldozes all emotions aside, including hope. Yet pain produces a bewildering range of ambivalence. While aspirin and paracetamol are the most commonly used drugs, and around one in five experience pain that has lasted longer than three months, so often we conspire to deny the reality of pain. We feel obliged to cheer the injured footballer who returns to the fray after losing teeth or being knocked unconscious. Many couples make a virtue out of refusing pain relief in childbirth. While a woman begs for an epidural, her husband gently counsels “remember we agreed … no drugs”. Many who have lived with pain tell of the scepticism of others (“You don’t look like you’re in pain”) but also of the subtle imperatives to stop their misery infecting those around them. Anglo and Asian women tend to be stoic in childbirth, while southern European and Arabic women are uninhibited in their expression. Moralists, including many in medicine, have often denied the dying sufficient morphine, fretting that they might become addicted.
Recently, television allowed us to consider the abandoned Serbian torture chamber, where unspeakable degradations were wrought on its Kosovar captives. Torture is the active infliction of pain on its unwilling victims. Professor Michael Cousins, head of the Pain Management Research Centre at Sydney’s Royal North Shore Hospital, describes unrelieved pain as “torture by omission”. The United Nations Declaration of Human Rights codifies civilised society’s most basic standards and aspirations for its citizens.
Yet as Cousins points out, the Declaration says nothing about the most elemental concern of all: the right to be relieved from pain.
This remarkable omission is a testimony to our ambivalence about pain. Its consequence is that pain management as a medical speciality lives a Cinderella existence, shining occasionally as islands of enlightenment in a sea of misery. The most recent and exciting developments involve discoveries about the way that damaged nerve endings sprout pain fibres, the growth of which can be inhibited and so the pain controlled through drugs administered through surgically implanted mini pumps. People who have lived for years in desperate pain are now being assisted to live largely pain-free lives again through such developments. Yet there are only seven pain management training centres in Australia, and for all the pious political talk of the need for palliative care after the overturning of the Northern Territory euthanasia legislation, cruelly token budgets have found their way into health expenditure in the period since.
As historically unprecedented falls in fecundity, better living standards and the successes of public health combine to cause the age distribution of the world’s populations to balloon increasingly to the right of the graph, more people will live with the pain of chronic degenerative conditions and cancer. Despite this, the disabling and all-absorbing nature of pain often militates against its victims becoming potent advocates for pain relief to be declared a basic human right, and all that would flow from this. If Cousins’ and his colleagues’ mission were to succeed, what a gift to the world this would be.