[updated 25 Sept, 9 Oct 2019]
Public health professor Kamran Siddiqi from the University of York tweeted today about a conference presentation from Robert West, who apparently was arguing that e-cigarettes “are perhaps the only smoking cessation intervention that has triangulation of evidence of effectiveness from three types of research”” randomized controlled trials, observational studies and population trends.

Putting aside that there have been many RCTs, observational studies and analyses of population trends which have focused on nicotine replacement therapy and other smoking cessation interventions, what does this evidence of effectiveness show about e-cigarettes?
Randomised Controlled Trials
I commented in an earlier blog about an English RCT where ecigs were compared to nicotine replacement therapy in smokers attending stop smoking services (so a self-selecting group who all also received supportive quit counselling, something that does not occur in real world NRT or ecig use), E-cigs were superior to NRT, but that was not saying much because quit rates in both groups were low.
Very recently a New Zealand study compared 1124 e-cigarette naïve smokers motivated to quit smoking who had been allocated to three arms of an RCT with the principal outcome of carbon monoxide verified continuous abstinence from smoking when measured at 6 months after the trial commenced. The trial compared (1) those given nicotine patches plus an e-cigarette with nicotine (2) those given nicotine patches plus an e-cigarette without nicotine and (3) those given nicotine patches. All three arms were offered 6 weeks of telephone delivered behavioural support (something that only tiny fractions of smokers trying to quit in real-world situations ever avail themselves of) and received a median of 3 such sessions. Analysis was on an “intention-to-treat” basis (ie of all who started the trial, including those who dropped out or were lost to follow-up) not just those who were available for assessment at the end of the trial. All who dropped out were assumed to be still smoking.
The study found that
“35 (7%) participants in the patches plus nicotine e-cigarette group had carbon monoxide-verified continuous abstinence at 6 months compared with 20 (4%) in the patches plus nicotine-free e-cigarette group (risk difference [RD] 2·99 [95% CI 0·17–5·81]), and three (2%) people in the patches only group (RD 4·60 [1·11–8·09]).”
In other words, after six months 93% of the patches plus nicotine e-cigs group were still smoking; 96% of the patches plus nicotine-free e-cigs group had not quit; and 98% of the nicotine patches group were still smoking. So the “value added” by using nicotinised e-cigs was just 3%. The authors described the impact of the patches + nicotine e-cigs group as having attained “a modest improvement” in smoking cessation.
I cannot think of any prescribed drug used for any condition where the condition persisted after 6 months use for 93% of users and where anything but the language of failure would be used about such an outcome. Is there anyone who would hail a 93% failure rate for contraceptives, antibiotics, cholesterol lowering drugs, analgesia, malaria prophylaxis or anything else as even a modest success?
Observational studies
The most important observational data we have on what happens to smokers who use e-cigarettes in normal conditions of use in the real world comes from longitudinal cohort studies of randomly selected people across whole communities. In an earlier blog, I summarized what two such recent papers told us about e-cig use. I reproduce a section of that blog below.
In 2018, two particularly important papers were published by US researchers using the longitudinal PATH ( Population Assessment of Tobacco and Health) data set.
Let’s take a close look at what they found.
Coleman B et al, Tob Control 2018
This important report on transitions in the vaping and smoking status of a nationally representative cohort of American adults aged 18+ who use electronic cigarettes (EC) provides rich data that greatly advances our understanding of the natural history of EC use.
If we examine the report’s data and consider the net impact of vaping on the critical goals of having vapers stopping smoking and vaping non-smokers not starting to smoke, the findings are very sobering and should give strong reason for pause among those advocating e-cigarettes as a game-changing way of stopping smoking.
The study reported on transitions between participants’ responses at Wave 1 and Wave 2, obtained 12 months later. At Wave 2, of the cohort of 2036 dual users (EC + smoking) only 104 (5.1%) had transitioned to exclusively using ECs and another 143 (7%) had quit both EC and smoking for a combined total of 247 (12.1%) who had persistently quit smoking. Of the 896 exclusive EC users at Wave 1, 277 (30.9%) had stopped vaping at Wave 2.
So together, 524 out of the 2932 EC users (17.9%) followed from Wave 1 might be considered to have had positive outcomes at Wave 2 (ie: quitting smoking and/or quitting EC).
The other side of the coin however, shows that of the 2036 dual users at Wave 1, 886 (43.5%) relapsed to using cigarettes exclusively. In addition, among the 896 exclusive EC users from Wave 1, 109 (12.2%) had stopped vaping and were now smoking, with another 121 having resumed smoking as well as using EC (i.e. became dual users). Importantly, 502 of 896 (56%) exclusive e-cigarette users were those who had never been established smokers prior to using e-cigarettes. Alarmingly, of these 502 adults, 120 (23.9%) progressed from using only e-cigarettes to either dual use (54 or 10.8%) or smoking only (66 or 13.2%).
Taken together, 886 dual users in Wave 1 relapsed to become exclusive cigarette smokers in Wave 2, and 230 exclusive vapers in Wave 1 took up cigarette smoking in Wave 2 (dual use or exclusively cigarettes). Undoubtedly, these should be considered as negative outcomes.
The table below shows that for every person vaping at Wave 1 who benefited across 12 months by quitting smoking, there were 2.1 who either relapsed to or took up smoking. Most disturbingly, in this adult cohort nearly one in four of those who had never been established smokers took up smoking after first using EC. Concern about putative gateway effects of ECs to smoking have been dominated by concerns about youth. These data showing transitions from EC to smoking in nearly a quarter of exclusive adult EC users with no histories of established smoking should widen this debate to consider adult gateway effects too.

By far the largest proportion of those with negative outcomes are those dual users who relapsed to smoking (886 or 43.5% of dual users). As the authors noted in their discussion, many of these were infrequent EC users, possibly involved in transitory experimentation at Wave 1. If we add the 902 who were still dual using at Wave 2, then 1788 of 2036 dual users (87.8%) in this sample might be said to have been held in smoking (dual using or exclusive smoking) 12 months later compared to 12.1% dual users who may have benefited by using ECs.
Commercial interests in both the tobacco and EC industries would be more than delighted with these findings. However, from public health harm reduction perspective these results argue against EC being a revolutionary effective harm reduction strategy, and point to their far stronger potential to both recruit smokers and hold many smokers in smoking.
Benmarhnia T et al American Journal of Epidemiology 2018 DOI: 10.1093/aje/kwy129
In a second paper using the PATH data, the authors considered persistent abstinence (not using tobacco for more than 30 days). The red highlighted section of the table below shows that those smokers who used ecigs (called ENDS in the table) had the worst persistent abstinence all-tobacco quit rates of any group in the cohort (5.6% of those who were vaping at the Wave 1 survey and 3.7% of those who too up vaping between Wave 1 and Wave 2). By far the most successful all-tobacco quit rate was for “no aid used” (ie cold turkey or unassisted cessation) with 12.5%.
When we multiply these quit rates by the numbers of smokers using each quit method, the yield of persistent quitters is even starker (see the second table below derived from the data in the table immediately below).

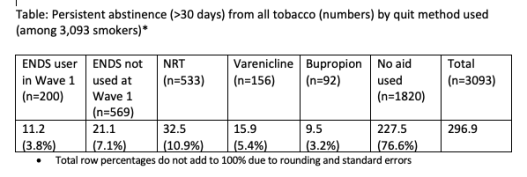
So in this major national cohort of US smokers, not only did EC use produce the lowest rate of persistent abstinence from tobacco use after one year compared to all other quit methods, but EC’s contribution to population-wide tobacco abstinence was utterly dwarfed by all other methods (10.9% v 89.1%). The much-denigrated and neglected unassisted cessation approach quietly ploughed on, continuing its massive historical dominance of how most ex-smokers quit, contributing 1.5 times more quitters than all other methods combined.
Population data
The Smoking in England Toolkit (STS) project (led by Robert West) provides wonderful data on the apparent associations between the downward trend in smoking prevalence in England since the study began in November 2006 through to recent months (see graph below). The dramatic upsurge in smokers using e-cigarettes in quit attempts that commenced in late 2012 and has more-or-less plateaued since mid 2013 does not appear to have had any marked impact on the slope of the historically declining smoking prevalence rate.

West co-authored an important report in late 2017 where they looked at whether the surge in e-cigarette use in England and whether this was reducing the number of cigarettes being smoked at the population level across the country. Their conclusions?
“No statistically significant associations were found between changes in use of e-cigarettes (â −0.012, 95% CI −0.026 to 0.002) or NRT (â 0.015, 95% CI −0.026 to 0.055) while smoking and daily cigarette consumption. Neither did we find clear evidence for an association between e-cigarette use (â −0.010, 95% CI −0.025 to 0.005 and â 0.011, 95%–0.027 to 0.004) or NRT use (â 0.006, 95%–0.030 to 0.043 and â 0.022, 95%–0.020 to 0.063) specifically for smoking reduction and temporary abstinence, respectively, and changes in daily cigarette consumption.
Conclusion If use of e-cigarettes and licensed NRT while smoking acted to reduce cigarette consumption in England between 2006 and 2016, the effect was likely very small at a population level.”
These findings echoed West’s comments to the BBC nearly two years earlier.

Two of the main pillars of the case made for e-cigarettes by their advocates are that they are a game-changing, disruptive technology which are powerful ways of quitting and dramatically cutting down the number of cigarettes smoked. The evidence above gives a rather complexion to such over-blown hype.
Meanwhile, data on the association between the changing affordability of smoking and smoking rates across the same period that e-cigarette sales have been rising offers a rather different picture, (see for example, UK data below)


Good to see a proper review of the evidence rather than the biased interpretation of mediocre findings presented by those now heavily invested in proving ecig efficacy.
LikeLike