[updated 29, 30 Sep, 15 Nov 2019, 18 Nov 2020] Advocates for e-cigarettes often appear to display cult-like adherence to a set of beliefs. Like beings possessed of inviolable truths, they repeat these as often as possible. Here are 12 articles of vaping faith, and why they are highly questionable.
- E-cigarettes are 95% less harmful than smoking
The “95% less harmful” claim was first made in a 2014 report chaired by Professor David Nutt, notable and perhaps unique in publicly declaring that e-cigarettes are “the most significant advance [in medicine] since antibiotics” , would be “the greatest health advance since vaccinations.” and that “to reject the opportunity of tobacco harm reduction is, perhaps, the worst example of scientific denial since the Catholic Church banned the works of Copernicus in 1616“, Seriously. The report was written by a selected group of 12 individuals who each were asked to estimate the relative harmfulness of e-cigarettes and other nicotine containing products compared to cigarettes. Their Big Number was repeated in a 2014 report by Public Health England, which again endorsed it in a 2015 update where it once again cited the Nutt report as a source, but again provided no transparent workings of how this figure was actually calculated. This is all PHE deigned to tell us in 2015:
“It had previously been estimated that EC [electronic cigarettes] are around 95% safer than smoking [10, 146]. This appears to remain a reasonable estimate.”
Reference #146 in the above update stated “The precise extent of harm from long-term use is not known but has been estimated at around 1/20th that of smoking tobacco cigarettes (5)” with the reference supporting that statement being – you guessed it – the Nutt report!
In its 2018 updated review PHE nudged the 95% even further toward certainty by slipping in “at least”:
“Vaping poses only a small fraction of the risks of smoking and switching completely from smoking to vaping conveys substantial health benefits over continued smoking. The previous estimate that, based on current knowledge, vaping is at least 95% less harmful than smoking remains a good way to communicate the large difference in relative risk unambiguously so that more smokers are encouraged to make the switch from smoking to vaping.”
The 2016 report of the Royal College of Physicians had this to say about the 95% less harmful figure:
“An analysis based on expert opinion quantified the likely harm to health and society of e-cigarettes at about 5% of the burden caused by tobacco smoking,(112) and a recent report by Public Health England supported this conclusion.(113)With appropriate product standards to minimise toxin and contaminant exposure in e-cigarette vapour, it should be possible to reduce risks of physical health still further. It is also possible, although unlikely, that other, unexpected harm from inhaling e-cigarette vapour over the longer term might yet emerge. Although it is not possible to quantify the long-term health risks associated with e-cigarettes precisely, the available data suggest that they are unlikely to exceed 5% of those associated with smoked tobacco products, and may well be substantially lower than this figure.” (p84)
“There appear to be few, if any, significant short-term adverse effects of e-cigarette use, but adverse health effects from long-term exposure to constituents of vapour cannot be ruled out. Although unknown, the hazard to health arising from long-term vapour inhalation is unlikely to exceed 5% of the harm from tobacco smoke.” (p185)
Reference 112 cited by the RCP was, yet again, the Nutt report. Indeed, all roads from the 95% estimate since 2015 have led back again and again to the Nutt report, or in the case of the PHE 2018 update, to no references at all tied to the calculation.
But what did the Nutt report itself say about its now famous number? Critically, the Nutt group conceded that “A limitation of this study is the lack of hard evidence for the harms of most products on most of the criteria”.
In 40 years of academic life in public health, and after editing a research journal (Tobacco Control) for 19 of these, I don’t ever recall reading such an eviscerating “actually, we have no evidence” caveat about the foundations of a supposed scientific risk assessment.
Despite this most sweeping and fundamental of caveat emptor statements about the lack of hard evidence, a senior Public Health England official told an Australian Parliamentary inquiry in October 2017 that “We are very clear that this is just one of the figures that we have used, and there are plenty more. We say what really matters is the evidence underlying this figure from the Nutt report”. (my emphasis).
So where then, is this “what really matters” underlying evidence which is not cited in the Nutt report nor in Public Health England’s reports? Where can we read and critically appraise the calculations that tipped the figure out into the ether?
Certainly in this video where Martin Dockrell of Public Health England explains how the magic number was conjured, there’s no reference to anything other than the consensus process used by the assembled Nutt meeting invitees, of which he was one.
Interviewer: Describe for us the evidence in the report and what is the science behind the 95% less harmful determination.
Dockrell: “…95% less harmful or 5% of the harm is a good way of expressing that – that subsequently appeared in the Royal College of Physicians report, It first appeared in a report published in 2014. It was led by Professor David Nutt. And David had done this kind of study before where it was a professional consensus process where you get a bunch of experts in the room. .. and we looked at what data we had for example on fires … we looked at what evidence we had about cancer risk and toxicant exposure and we had some data on that. And on the basis of the data we had [describes which nicotine containing products were compared] ..them the computer churns out a figure and we see .. e-cigarettes coming out at 5% of the risk…
Interviewer: You’ve got the 5% of potential harm … how conservative is that? Like if you were to go through everything today would it be the same number?
Dockrell: Well we published that study 5 years ago and now we have 5 years, more than 5 years more data. We have these excellent biomarkers studies. We know much more about e-cigarette vapour and how that might effect bystanders — not at all is the shorthand for that one. And so, yeah it would depend on the experts you got around the table [my emphasis] but I think that looking at the data that we’ve got even it would be less than 5%. It would be substantially less than 5%.”
A factoid is “an item of unreliable information that is repeated so often that it becomes accepted as fact.” The “95% safer” statement is nothing but a factoid that has attained an almost Trumpian-like resonance. It is an emperor with suspiciously few clothes.
[Addendum: in 2020 I co-authored this critique of the “95% safer” factoid Eissenberg T, Bhatnagar A, Chapman S, Jordl S-E, Shidadeh AZ, Soule E. Invalidity of an oft-cited estimate of the relative harms of electronic cigarette. Am J Public Health 2020; 110(2) 161-2]
- We don’t know the long-term effects of vaping but toxicology has advanced massively in past decades, so it’s not too early to now call e-cigarettes as all-but-safe
Cigarette use exploded at the beginning of last century after mechanisation replaced handmade cigarettes, making smoking very affordable. But tobacco-caused diseases didn’t start showing up in larger numbers until 30-40 years later. The US surgeon Alton Oschner, recalling attendance at his first lung cancer autopsy in 1919, was told he “might never see another such case as long as we lived”. He saw no further cases until 1936 — 17 years later – and then saw another nine cases in six months. Today lung cancer is (by far) the world’s leading cause of cancer death.
The incidence of lung cancer rose rapidly in the decades 1930-1980 but it was not until 1950 that seriously compelling evidence was published in the USA and the UK that long-term smoking caused lung cancer. Knowledge about smoking’s causal role in other diseases followed.
If any scientist had declared in 1920 that cigarette smoking was all but harmless, history would have judged their call as dangerously incorrect. But this is the doctrinaire call that many vaping advocates are making regularly today, after just 10 years of use.
With vaping only having been around in large numbers for about ten years, it is predictable and unsurprising that we have as yet seen little clinical disease presenting from e-cigarette vaping, although the recent growing numbers of deadly serious respiratory diseases now appearing in the USA may be an early canary in this coalmine.
The recent New England Journal of Medicine report of serious pulmonary disease in two states in 53 vapers with a median age of just 19, found that 17% of these patients reported vaping only nicotine products. British vape advocates have been quick to point out that none of these cases are occurring in the UK. Oh … wait … hold the press. Here’s a case-report just in.
When many have pointed out this fundamental “too soon to know” problem, vaping defenders argue that toxicological science has progressed exponentially, with the implication being that we can now tell very early with a high degree of certainty if a drug or chemical is likely to cause disease down the track.
That would be all that advanced crystal-balling toxicology capable of detecting long term risk so brilliantly that between 1953-2014, 462 drugs initially assessed as being likely to be safe and let into the market have been withdrawn with some causing death, or very serious health problems. Remember thalidomide?
A reason why we have Therapeutic Goods Administration drug assessment, scheduling, adverse event reporting and the possibility of recall and bans is because pre-registration drug trials can never provide data on the consequences of long term use. In 2017 vaping activists were jubilant about a 3.5 year follow-up study of just 9 subjects (with another 7 having dropped out) which, hey presto, showed no “long term” ill-effects. “Case closed: study shows no lung damage from vaping” screamed one report.
This baby-steps follow-up compares with the 30-40 years that passed before the huge upswing in smoking in the first decade of the twentieth century began to show lung cancer in case control studies in the early 1950s.
The recent door-stopper report on e-cigs of the US National Academies of Sciences, Engineering and Medicine found:
- There is substantial evidence that e-cigarette aerosols can induce acute endothelial cell dysfunction, although the long-term consequences and outcomes on these parameters with long-term exposure to e-cigarette aerosol are uncertain.
- There is substantial evidence that components of e-cigarette aerosols can promote formation of reactive oxygen species/oxidative stress. Although this supports the biological plausibility of tissue injury and disease from long-term exposure to e-cigarette aerosols, generation of reactive oxygen species and oxidative stress induction is generally lower from e-cigarettes than from combustible tobacco cigarette smoke.
- There is substantial evidence that some chemicals present in e-cigarette aerosols (e.g., formaldehyde, acrolein) are capable of causing DNA damage and mutagenesis. This supports the biological plausibility that long-term exposure to e-cigarette aerosols could increase risk of cancer and adverse reproductive outcomes. Whether or not the levels of exposure are high enough to contribute to human carcinogenesis
Reckless calls to just allow unregulated e-cigs to flood corner stores and be promoted with advertising like this https://twitter.com/SimonChapman6/status/970366837719314432 promising “risk free” vaping and within one corker of a self-contradictory sentence, that vapers can “entirely avoid the harm” while “lessen[ing] the possibility of inducing danger on your lungs” is the sort of world we are supposed to embrace by these flatulent arguments.
If e-cigs are so safe and so effective, their manufacturers surely have nothing to fear by applying for registration through the Australian Therapeutic Goods Administration. Why is it then, that no such applications have apparently been received? What might these manufacturers know or fear that the TGA might conclude?
- Nicotine is all but benign. It’s cigarettes that cause all the harm
Like pilgrims at a religious shrine, vaping advocates also have cult-like veneration for a statement by the late addiction research Michael Russell who stated in 1976 that “People smoke for the nicotine but they die from the tar”.
Since Russell made that statement a whole 43 years ago there has been an extensive body of evidence published suggesting that nicotine, while not being carcinogenic, is a tumour promoter. For example:
“Although nicotine itself is regularly not referred to as a carcinogen, there is an ongoing debate whether nicotine functions as a ‘tumour promoter’. Nicotine, with its specific binding to nAChR, deregulates essential biological processes like regulation of cell proliferation, apoptosis, migration, invasion, angiogenesis, inflammation and cell-mediated immunity in a wide variety of cells including foetal (regulation of development), embryonic and adult stem cells, adult tissues as well as cancer cells. Nicotine seems involved in fundamental aspects of the biology of malignant diseases, as well as of neurodegeneration.”
This 2015 review of research relevant to nicotine and the adolescent brain looked at “how acute exposure to nicotine impacts brain development and how drug responses differ from those seen in adults.” The authors discussed “the persistent alterations in neuronal signaling and cognitive function that result from chronic nicotine exposure, while highlighting a low dose, semi-chronic exposure paradigm that may better model adolescent tobacco use” and argued “that nicotine exposure, increasingly occurring as a result of e-cigarette use, may induce epigenetic changes that sensitize the brain to other drugs and prime it for future substance abuse”.
Those like John Britton still asserting in 2019 that long term use of nicotine represents a health risk similar to coffee consumption might like to dive a little deeper into the toxicological literature on nicotine.
- The thousands of flavouring chemicals used in vape juice have all been declared safe by regulators

There are now some 8000 beguiling and often child-friendly flavours being sold in e-juice [Allen et al, 2016; Barrington-Trimis et al, 2014]. Many of these have been approved for ingestion as food additives, but have never been approved for inhalation. The U.S. flavouring industry has said about this important difference:
“The manufacturers and marketers of ENDS [electronic nicotine delivery systems], and all other flavored tobacco products, and flavor manufacturers and marketers, should not represent or suggest that the flavor ingredients used in these products are safe because they have FEMA GRASTM status for use in food because such statements are false and misleading”
Science journalist Dr Heather Goldstone put it beautifully like this (at 11m10to 24m50)
“It doesn’t take someone with an advanced degree in toxicology to understand that drinking water is different than breathing water”.
So beware of fake news that inhaling #vaping flavourants are benign because many used in food flavouring.
For some flavourants, for example cinnamon, there is already evidence for cytotoxicity [Behar et al, 2014] and for the very commonly utilised additive diacetyl, which produces a pleasant, buttery taste in e-liquid, there is an association with the causation of the non-reversible respiratory condition Bronchiolitis Obliterans [Farsalinos et al, 2015]. The English Cherry flavoured vaping fluids have also been demonstrated, via the inhalation of the irritant benzaldehyde, to be a potential concern for long term users [Kosmider et al, 2016].
Our knowledge of the impact of long-term inhalation, on average 200 times a day (and up to 600) over many years in daily vapers, of vapour arising from the heating of these chemicals is in its infancy.
- Many smokers have greatly reduced the number of cigarettes they smoke daily: this is no-brainer harm reduction in action!
If you smoke 20 cigarettes a day, and vaping sees you reduce this by half, surely anyone with half a brain can understand that this means you will have greatly reduced your risk of disease and death from smoking? But counter-intuitive as it seems, this is not what the evidence shows. Cohort studies which have followed large numbers of smokers for years have found that those who cut back the number of cigarettes they smoke but do not quit, experience negligible reductions in mortality.
A Norwegian cohort of 51,210 people followed from the 1970s until 2003 found “no evidence that smokers who cut down their daily cigarette consumption by >50% reduce their risk of premature death significantly.” A Scottish study of two cohorts followed from the 1970s to 2010 found no evidence of reduced mortality in reducers, but clear evidence in quitters and concluded “that reducing cigarette consumption should not be promoted as a means of reducing mortality.” The largest study, from Korea and involving 479,156 men followed for 11 years, found no association between smoking reduction and all cancer risk but a significant decrease in risk of lung cancer, with the size of risk reduction “disproportionately smaller than expected”.
As illustrated in the table below, when randomly selected groups of vapers are followed up at 12 months, by far the most common outcome is that those who were smoking and vaping at the beginning of the 12 months study period will still be vaping and smoking at the end of the 12 months. That might suggest that the vaping holds far more in smoking than it tips out of it.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6202279/pdf/nihms965122.pdf
Also, studies of the number of cigarettes foregone by dual-using vapers have shown that compared with smokers who never vape, that average daily cigarette consumption is little different. See for example below:
- Secondhand vape is harmless and nothing to worry about
Our knowledge of the harms of secondhand smoke comes almost entirely from studies of non-smokers who live with smokers and those who worked in enclosed environments where smoking was allowed. While it is true that e-cigarette emissions are far less than those from combusted tobacco, they are very much not the equivalent of water vapour from a kettle, as a senior Philip Morris official recently tweeted (below). Vape consists of vapourised propylene glycol or vegetable glycerine, nicotine, flavouring chemicals and often tiny metal particles (chromium, nickel and lead) shed from the heated metal coil in vaping equipment.
Vape advocates argue, in all seriousness, that we should all be happy to allow vaping in all indoor spaces because this will discourage vapers from going outside and joining smoker where they might relapse back into smoking. As I wrote in a debate
“Another argument used by indoor vaping advocates is that indoor vaping bans will cause former smokers who now vape to go outside, where exposure to sensory cues from exiled cigarette smokers will trigger their relapse back to smoking. This would be all the fault of non-smokers selfishly putting their own health and comfort ahead of vapers and contributing to their stigmatisation. By this argument non-smokers should be happy to be exposed to ambient vape in aircraft, workplaces, restaurants and bars (or even sustained clouding sessions) to make e-cig users feel more “included” and in the hope that they might quit smoking.”
Importantly, vapers often gather together in social groups where they billow clouds of vape into the air producing particle concentrations comparable or greater to that found in bars when smoking was permitted. Vaping advocates want to wind the clock back and start fighting the same arguments that were won long ago over secondhand smoke exposure.
- E-cigarettes are a very effective way to quit smoking
There’s no shortage of individuals who swear blind that they had tried all sorts of ways to quit smoking until vaping worked for them. This is true for those individuals, just as there are success stories with methods of quitting like acupuncture, and hypnotherapy which have poor outcomes when assessed by principles of evidence-based medicine. In this recent blog of mine, I summarized recent evidence from randomized control trials, cohort studies and national population data, the three most important sources of information.
In a recent RCT from New Zealand, after six months 93% of the patches plus nicotine e-cigs group were still smoking; 96% of the patches plus nicotine-free e-cigs group had not quit; and 98% of the nicotine patches group were still smoking. The authors described the impact of the patches + nicotine e-cigs group as having attained “a modest improvement” in smoking cessation over patches alone.
I cannot think of any prescribed drug used for any condition where the condition persisted after 6 month use for 93% of users and where anything but the language of failure would be used about such an outcome. Is there anyone who would hail a 93% failure rate for contraceptives, antibiotics, cholesterol lowering drugs, analgesia, malaria prophylaxis or anything else as even a “modest” success?
- There are many smokers who just can’t quit, so we need e-cigarettes to help them
This claim derives from the so-called hardening hypothesis which states that, as smoking prevalence falls ever lower, the remaining smokers will be die-hard addicted “refractory” smokers who just can’t quit. They are impervious to the suite of tobacco control policies and campaigns that have driven hundreds of millions of smokers around the world to quit. It’s time we acknowledged that these smokers just can’t quit and so we are condemning many of them to death if we don’t put policies in place that will help them quit smoking with e-cigs. To do anything else would be unethical, they try to argue.
Aside from the dismal evidence referred to earlier that e-cigs are pretty hopeless in helping people quit, the entire premise of the hypothesis is an evidence-free house of cards.
Whenever this hypothesis has been tested against the evidence it has been found wanting. In nations or states where smoking prevalence has fallen most, one would expect (if the hardening hypothesis was correct) that indices of hardened smokers (such as mean number of cigarettes smoked per day) would be rising because the remaining smokers would be over-represented by heavy, addicted smokers.
Unfortunately for this argument, John Hughes, one of the world’s most respected and prolific researchers on smoking cessation, recently let all the air out of the hardening hypothesis tyres in a paper in Nicotine and Tobacco Research. He reviewed 26 studies on hardening and found:
“None of the 26 studies found that conversion from current to former smoking, number of quit attempts, or success on a given quit attempt decreased over time and several found these increased over time.” He concluded “Some have argued that a greater emphasis on harm reduction or intensive treatment approaches is needed because remaining smokers are those who are less likely to stop with current methods. The current review finds no or little evidence for this rationale.”
- Countries with lots of vaping have lower smoking rates than those which don’t. Look at England! Vaping has rapidly supercharged the fall in smoking
As at September 2019, the latest available data on smoking prevalence among five anglophone nations which are often compared shows that Australia and the UK are level pegging at 15.1% as nations with the lowest smoking prevalence.
- Australia (2017-18 ages 18+): 15.1% (this figure includes cigarette and roll-your-own smokers plus all exclusive users of other combustible tobacco products like pipes, cigars, hookah and shisha)
- USA: (2017 ages 18+) 16.7% (like Australia, includes all combustible tobacco product users)
- Canada (2017 ages 12+): 16.2% (cigarettes & Roll Your Own tobacco only)
- New Zealand (2016 ages 15+) 15.7%. (Māori adults 35.3%) (cigarettes & RYO only)
- UK (2017 ages 18+): 15.1% (cigarettes and RYO only)
Most recently Victorian data on changes in smoking prevalence in that state between 2015-2018 show the lowest daily smoking prevalence ever recorded: 10.7% (down from 13.5% in 2015) with falls in the most disadvantaged group down from 16.8% to 13%.
In summary, of these five nations, only Australia and the USA include all combustible tobacco products in their data on “smoking” prevalence, while other nations only include cigarettes (factory made and hand-rolled). The “smoking” prevalence figures from Canada, New Zealand and the UK thus underestimate the true prevalence of “smoking”. Australia and the UK have the same (lowest) prevalence of these nations, although UK data does not include combustibles (cigars, pipes, shisha) other than cigarettes. It is therefore likely that Australia has the lowest smoking prevalence. Yet it has the lowest prevalence of vaping and the most restrictive e-cigarette policies. You can go many days without ever seeing anyone vaping in Australia.
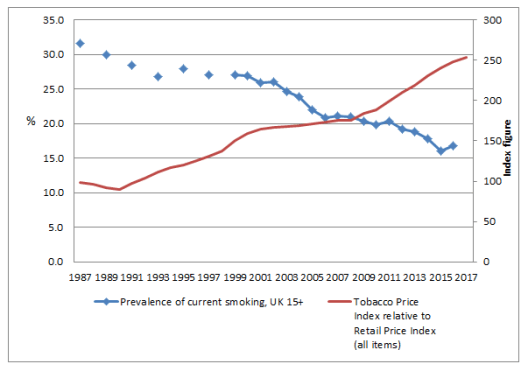
Vaping advocates argue that nations with widespread vaping are seeing their falls in smoking prevalence accelerate because of vaping. Just this month, the UK’s John Britton argued that while “it would be premature to attribute these differences in smoking trends solely to differences in electronic cigarette policy” that “the figures do suggest that the UK approach of medical endorsement with marketing controls and product regulation has to date succeeded in harnessing the potential of electronic cigarettes to significantly accelerate the decline in adult smoking prevalence.”
Data from the Smoking in England project in the graph below show that the role of e-cigarettes in accelerating the downward trend in England is far from obvious or significant. The dramatic upsurge in smokers using e-cigarettes in quit attempts using e-cigarettes that commenced in late 2012 and has more-or-less plateaued since mid 2013, does not appear to have had any marked impact on the slope of the historically declining smoking prevalence rate.

An important report from late 2017 considered the surge in e-cigarette use in England and whether this was reducing the number of cigarettes being smoked at the population level across the country. The conclusions?
“No statistically significant associations were found between changes in use of e-cigarettes while smoking and daily cigarette consumption. Neither did we find clear evidence for an association between e-cigarette use specifically for smoking reduction and temporary abstinence, respectively, and changes in daily cigarette consumption. If use of e-cigarettes and licensed NRT while smoking acted to reduce cigarette consumption in England between 2006 and 2016, the effect was likely very small at a population level.”
Robert West is a world leader in smoking research, and the editor-in-chief of the journal Addiction. He told the BBC in 2016
“[This widespread use of e-cigarettes] raises an interesting question for us: If they were this game changer, if they were going to be – have this massive effect on everyone switching to e-cigarettes and stopping smoking we might have expected to see a bigger effect than we have seen so far which has actually been relatively small” [my emphasis]
However, if we look at the data on smoking prevalence and changes in smoking affordability in the UK, we can see a rather different picture.
- There are very few health agencies which don’t unequivocally support vaping and “light touch” e-cigarette regulation
Oh really? If you’ve got half an hour to spare, take a tour through this list of 46 global, regional and national agencies who very much beg to differ. The list Includes the World Health Organization, the US National Academies of Science, Engineering and Medicine, and just about every major US and Australian health agency.
- Big Tobacco is a minor player in the global vaping business
Vaping advocates like to paint pictures of plucky, noble start-up minnow vaping companies valiantly “game changing” the nicotine addiction landscape. “Big tobacco is not at the leading edge of either product innovation or sales” they protest. And in Australia, they point out that none of the transnational tobacco companies are selling their products here … yet.
The history of transnational tobacco company take-overs of profitable smaller tobacco companies shows us that the transnational companies gobble up all profitable or threatening small companies whenever they can. The same pattern is rapidly emerging with e-cigarettes.
Altria, which sells Marlboro in the USA, has bought 35% of Juul. This article describes the take-over of the e-cigarette market by Big Tobacco. All of these companies continue to resist and attack effective tobacco control policies, while posturing about caring about harm reduction.
- Tobacco companies are doing all they can to reduce smoking in concert with their efforts to promote vapourised nicotine products
Philip Morris International currently has a global “unsmoke” campaign trying to convince us all that it really, really wants all its customers to switch from cigarette to its putative reduced harm vapourised product, IQOS. In the tweet below it even profiled Bryan, a smoker who had given up all nicotine too! That’s right. Philip Morris has broken out the maypole and has all its employees and shareholders dancing around it each lunchtime because the company is doing all it can to get all its customers off all its products and publicly broadcasting its success stories!
 I
I
But the company has set no targets for its reductions and around the world. It’s business as usual trying to maximise sales of its cigarettes and its IQOS heat not burn product. It has its foot-to-the-floor promoting cigarettes in every market and doing what it can to oppose effective tobacco control which would actually reduce smoking. Here are ten questions I put to Philip Morris about this sham, their reply, and my response.

Superb stuff, Simon. You may not be uni teaching anymore, but sure as hell giving out good lessons.
Pretty sure a big typo
LikeLike