Tags
Across my career, I’ve often been asked by media interviewers “What got you involved in the sort of work you do? What drives you to keep at it?” Depending on who’s asking, there’s an occasional edge to the questions presaging that a little probing will lift the lid on a deep moralistic busybody, driven by a barely disguised missionary zeal to lead sinful smokers off the pernicious path of self-destruction and into a wholesome life of glistening health.
In the 1970s, when I first started working in health, I’d sometimes sense the same assumptions in people I talked to at parties. When they asked “what do you do?” and I answered that I worked in tobacco control, I’d often sense the hesitancy: he probably doesn’t drink. Never smoked dope. No chance of any fun or sex with this guy. He probably thinks the music’s too loud. Steer well clear.
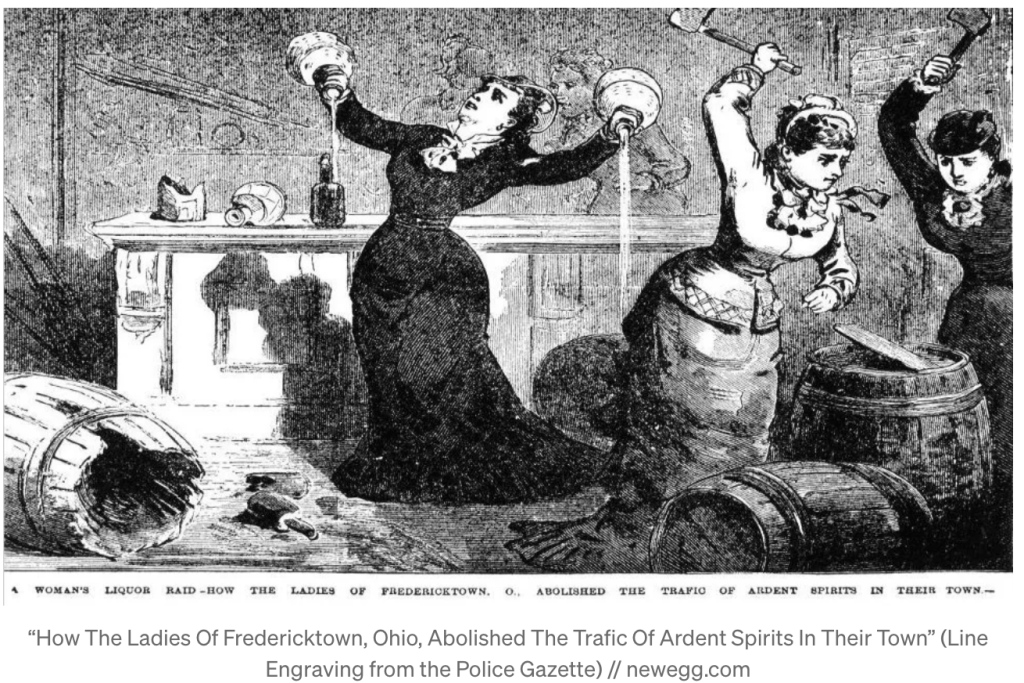
Early anti-smoking efforts in the years before strong evidence rolled out in the early1950s that smoking was deadly were deeply mired in puritanism and ideas that the body was a temple from which the devil and his work had to be driven out. The evils of drink, smoking, masturbation, temptresses and reading novels travelled together in a morals crusade that extoled abstention from fun and pleasure. Purse-lipped temperance groups picketing pubs, jokes about Methodists who eschewed dancing and the rest, and the way that smoking and under-age drinking were pretty reliable markers of kids who were often more edgy and interesting than their heads-down classmates all coalesced in those early days to make any mention of tobacco control a tad suspect.
When the Niagara of evidence became undeniable that smoking was out on its own as a cause of disease affecting almost every part of the body, the moralists’ chorus was joined by doctors and health authorities who had long also brought us warnings about other dangers that we were thankful to receive. Just as no-one thinks of a lifesaver at the beach warning about sharks or dangerous rips as a moralist or killjoy, the overwhelming evidence that smoking was harmful radically changed the complexion of anti-smoking efforts. This became ethically turbo-charged when strong evidence emerged that chronic exposure to other people’s tobacco smoke was also deadly.

Seventy four years along from these early studies, research has repeatedly confirmed that around 90% of smokers regret ever starting. While some die-hard smokers still want to trot out their favourite talismanic self-exempting beliefs (“plenty of people smoke all their lives and don’t die early”, “everything’s bad for you these days”, “what about all the air pollution we breathe on every day?”, “I keep fit, so get the nasty stuff out of my system”), and some insist that smoking is pleasurable, most smokers today are reluctant, embarrassed and apologetic. A huge majority have tried to quit and I’ve never met a smoker who hoped their children would take it up. There are few — if any — products with such a near-universal disloyalty and resentment among their consumers.
Most occupations and professions don’t attract the sort of questioning I described earlier. I can’t imagine ever saying to an accountant “so what was it that got you interested in accounting when you started?” or asking a dry cleaner “you’ve been doing this for 35 years … can I ask what the fascination is?” We mainly assume that it’s the money, the security and comfortable routine, inertia and the quality of working environments that keeps people in their jobs or attracts them into something else.
We don’t think to ask surgeons or oncologists why they do what they do. It’s obvious that people likely to die from cancer often desperately want to try and avoid that happening, or give themselves some extra time. But it’s also obvious that most people need little convincing that prevention is as, or more important than curing or treating. Yet while the thought of people railing against the work of lung cancer surgeons is unthinkable, all across my career I’ve seen bizarre and sad little pro-smoking and more recently pro-vaping groups form, flutter and fade and heard smokers calling radio programs to whine about feeling under siege.
The “explain yourself” imperative is generally reserved for those who choose to do odd, anti-social, demanding, revolting, seamy or dangerous work: undertakers, midnight to dawn radio hosts, sex workers, plumbers who wade in raw sewage, skyscraper window cleaners. With daily smoking prevalence in Australia down to 8.4%, and 90% of smokers regretting ever having started and often highly supportive of polices that might help them smoke less or quit, we are looking at a mere 0.8% of the adult population who are contented and committed smokers, with even a smaller proportion of these actively railing against tobacco control. Fringe political parties in Australia which have sometimes run candidates have received derisory public support.
So when I’m occasionally asked the “why?” question these days, that perspective on the likely attitudes of those listening to the interview (it’s usually on radio) guides my response. I’m never tempted to try and repudiate the time-warped, neo-puritanical framing of the question as if it’s a serious, widespread critique. Instead, I steer the conversation over to considering the importance of and challenges in hobbling and discrediting the upstream well-heeled forces that keep promoting smoking and doing all they can to defeat, dilute and delay effective tobacco control policies capable of reducing smoking on a wide scale.
I’ve worked in public health since late 1974. I’ve focussed on a range of issues that extend from tobacco control, gun control, helping people better understand the risks and benefits of adopting (or avoiding) certain medical procedures such as having prostate specific antigen test or getting immunised) or avoiding (or not) exposure to allegedly “dangerous” technology like mobile phones and transmission towers and wind turbines.
The common thread in most of these issues are the efforts of industries, lobby groups and determined, often obsessed individuals to thwart evidence-based public health policy and practice which threatens these industries or the cult-like belief systems of people who eat, live and breathe hatred of a public health strategy. This hatred has a very long history (see below).

A classic analytical matrix in public health (Haddon’s matrix) is the epidemiological triad that was first applied to the effort to understand and then better control road injury and later infectious and vector-borne diseases like cholera and malaria: the agent, host, environment and vector matrix.
In the control of malaria, we put a lot of effort into understanding the agent that causes the disease, the five types of plasmodium parasite that multiply in human red blood cells of humans and in the mosquito intestine. Agent control involves efforts to develop a vaccine which would prevent a person being bitten by a mosquito carrying the parasite from developing malaria. One such vaccine first passed human trials in 2017, possibly indicating a revolution in efforts to control this terrible disease.
Those who are infected with the plasmodium parasite are known as “hosts”. Here, control efforts are concerned with educating those who live in areas where malaria is endemic to take efforts to protect themselves from being bitten by covering-up at times when they are most likely to be bitten, wearing repellent, using insecticides and being diligent about destroying or spraying mosquito breeding water like that which collects inside old tyres, cans, and water storage. These breeding areas are known as the “environments” that need to be mapped, inspected and controlled. A wider definition of environments would embrace considerations of the cultural, economic and political environments in endemic malaria areas. If local health authorities had no funds to support malaria control, this would be importantly identified in a malaria control analysis and efforts taken to raise such funding and support.
Finally, the female anopheles mosquito is known as the “vector” responsible for the plasmodium parasite agent entering the bloodstream of hosts. Vector control starts with studying the life-course and behaviour of these insects in attempts to wreck their efforts to bite people.
Big Tobacco: the global vector for lung cancer
In tobacco control, the vector whose every waking moment is concerned with maximising the number of smokers (hosts) who consume tobacco (the agent) is the tobacco industry. So a large part of my work across 40 years has been involved in exposing and shaming the industry, its acolytes and those in politics who take its donations and hospitality, oppose or water down potent legislation and collude with its ambitions to keep as many people smoking as possible.
The “what has kept you going in this issue all these years” question is easily answered in two ways. First, smoking rates in both adults and kids are at all-time lows, and showing no signs of not falling even further. Lung cancer, a rare disease at the beginning of the twentieth century, rose to become the leading cause of cancer death by the 1960s. But in Australia, male lung cancer rates stopped rising in the early 1980s and have continued to fall, some 30 years after we first saw large-scale quitting happening about the huge publicity was given to the bad news about health. Female lung cancer rates look to have plateaued at a level that makes their peak just a few years ago reach only half the peak rates that men reached over 30 years ago.
Continually falling disease and death rates from tobacco caused diseases have made tobacco control the poster child of chronic disease control, envied by people working today in areas like obesity and diabetes control. It’s been such a privilege to have contributed to many of the major policy developments that have happened since the 1970s: advertising bans, the highest priced cigarettes in the world, large scale quit campaigns, smoke free legislation in workplaces, bars and restaurants, plain packaging, graphic health warnings on packs, bans on retail displays of tobacco products, and a duty free limit of just one pack.
Second, the mendacity of those working in the tobacco industry throughout my career has strongly motivated me to keep hard at it. In the decades before the evidence on tobacco’s harms were established, anyone working for the tobacco industry might have as easily been working for any industry. They were selling a product with strong demand and surrounded by convivial social rituals. The companies employed many people and contributed to communities via sponsorships and benefaction. What was not to like?
But with the advent of the bad news, the industry rapidly descended into decades of the very worst of corporate malfeasance. Those who stayed with the industry or came into it did so with their eyes wide open about what they were being rewarded to do every day and so were open game to account for their actions and the consequences. In the face of all they now knew, the industry doubled down. It conspired with other companies to deny the harms, it lied that nicotine was not addictive, shredded oceans of incriminatory internal documents, corrupted science through tame consultants and scientists, bribed politicians, promoted pro-smoking doctors to the media, donated to political parties likely to support its goals, bought up community support via vast sponsorship of national and international sport and culture, chemically manipulated cigarettes to make then more addictive, researched and targeted children in its advertising and promotions, relentlessly attacked any tobacco control proposal that threatened in any way to harm its bottom-line, cynically supported limp tobacco control policies that it knew were useless but made it look good, and supplied products to agents known to be involved in illicit, black market trade while unctuously railing against that trade in public, posturing as good corporate citizens.
The industry has long been peerless in occupying the tawdry throne of corporate ethical bottom feeders. This popular and political understanding is now so pervasive that its conduct has become an almost universal comparator for corporate pariah status. Big Tobacco is the index case here. If you google “just like the tobacco industry” you will be deluged by a rogues’ gallery of other industries that have lost public trust. The industry acknowledges that it today has serious trouble attracting quality staff.
Shining 10,000 watt arc lights on that conduct has been of immense importance to tobacco control. It is rare today to find a politician is who happy share a photo opportunity with any tobacco company. When I interviewed Australia’s former health minister and attorney general, Nicola Roxon, for my book (with Becky Freeman) about Australia’s historic adoption of plain packaging, she emphasised that “everyone hates the tobacco industry” and that this understanding had steeled the government to proceed and brace against the industry’s best efforts to defeat the legislation. That public revulsion did not develop out of nowhere – it was an important enabling objective for many of us in tobacco control in our advocacy for policy change.
All companies today are engaged in high profile rebirthing displays where they openly acknowledge that smoking is deadly and argue that they want to do all they can to encourage smokers and future smokers to switch to electronic vapourised nicotine products like e-cigarettes. After around 12 years of widespread use, they have declared that consensus already exists that these products are all but totally benign. More and more authoritative reviews of the evidence on this show this consensus is very far from the case and that they are far from magic bullets or “Kodak moment” game changers in helping smokers quit.
While spokespeople working down one corridor of tobacco companies extol the virtues of these new products and megaphone the transformational role they will play in the tobacco industry, those working elsewhere in the building continue to do all they can to attack proposals for effective tobacco control policies and legislation wherever they can. In recent years all the major companies have mounted huge efforts to try and stop plain packaging, graphic health warnings, increased tobacco taxation, retail display bans, and flavour bans. If they really wanted to see an end to smoking, they would aggressively advocate for all these policies. So go figure.
This blatant duplicity is stomach-churning. The industry’s clear goal is to not have its customers abandon cigarettes and use e-cigarettes instead. It is to have these customers use both products (known as dual use), to tempt former smokers back into nicotine addiction and to reassure teenagers that these allegedly safe as you can get products hold none of the threats that smoking holds. They cannot believe their luck.
The evidence is mounting that this scenario is exactly the way things are playing out. E-cigarette users are in fact less likely to quit than smokers not using them. And dual use is the most common pattern of use, often lasting years.
Every single policy in tobacco control that has ever been advocated by those of us working in this field around the world has been adopted in many nations. In Australia, the tobacco industry has lost every policy battle it ever fought. As a result, we have been able to get where we have in dramatically reducing smoking to the lowest levels ever recorded. Teenage smoking is almost extinct in Australia and several other nations. These are fantastic outcomes.
